A summary of: The Insulin & Heart Doctor with Dr. Pradip Jamnadas
Heart disease remains the number one killer worldwide, but the real culprits behind this epidemic may surprise you. Dr. Pradip Jamnadas, a world-leading cardiologist who has treated over 30,000 patients in his 35-year career, reveals shocking truths about what’s really causing heart attacks in increasingly younger people, and most importantly, how to prevent them through simple lifestyle changes.
The Cardio Paradox: Why Too Much Can Harm Your Heart
In a counterintuitive revelation, Dr. Jamnadas observes a disturbing pattern in his practice: “People who overly do aerobic activity … actually end up with more inflammation in their body, and they end up with more coronary artery disease than patients who do short sprints, and patients who do resistance exercises, and patients who do HIITs (high-intensity interval training).”
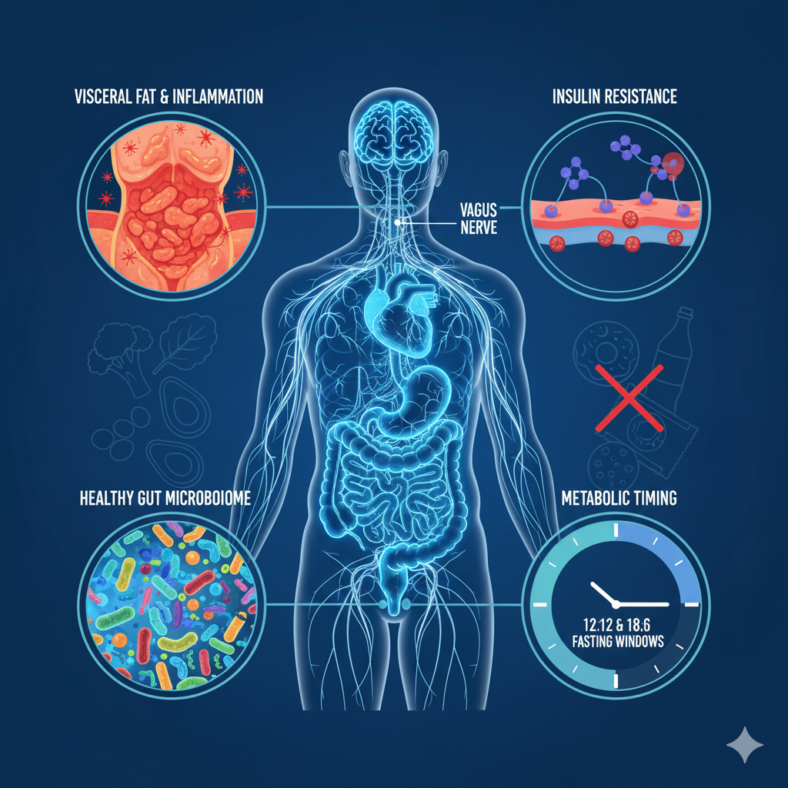
The mechanism behind this is fascinating. When you over-exercise, especially with prolonged aerobic activity, you divert blood from your gut to your muscles. This causes relative ischemia (lack of circulation) to your gut, which affects the enteric nervous system and the vagus nerve that ends in your gut lining. This disruption can trigger heart palpitations and contribute to systemic inflammation.
The recommendation? “You need some aerobic training,” Dr. Jamnadas explains, “because you want to develop some endurance… but you should only do a maximum of about 150 minutes of aerobic activity a week.” The sweet spot for heart health is combining moderate aerobic exercise with resistance training and HIIT workouts.
Breakfast and the Insulin Resistance Trap
The conventional wisdom about breakfast being “the most important meal of the day” deserves scrutiny through the lens of insulin resistance. Dr. Jamnadas explains the hidden danger: “If I’m eating every three hours and I’m consuming glucose or I’m consuming starchy foods or I’m consuming carbohydrates… I’m stimulating my pancreas. I’m stimulating my insulin. My insulin goes up, it comes down. But before it even gets a chance to come down, it goes up again.”
The problem isn’t just what you eat for breakfast, but the frequency of eating throughout the day. “The repeated consumption and frequent consumption of glucose is causing my insulin to stay high because insulin stays a little bit longer in the bloodstream than the glucose. The glucose will come down in about two to three hours, but the insulin stays higher for about four hours.”
This chronic elevation leads to insulin resistance: “Any hormone that stays in your body for a long time, the body becomes immune to it.” The downstream effects are devastating. By the time you’re diagnosed with diabetes, “you already have coronary artery disease.”
The Sleep-Gut-Heart Connection: One Bad Night Changes Everything
The importance of sleep extends far beyond feeling rested. Dr. Jamnadas delivers a stark warning: “One night of bad sleep, you become insulin resistant the next day.”
The mechanism involves the gut microbiome and the vagus nerve. “Sleep is absolutely important,” he emphasizes. “Lack of sleep causes a change in your gut microbiome. You’ve got to sleep seven hours a night. And cutting down on sleep is going to affect your entire physiology in your body and your repair processes and your vagus nerve and your delta sleep. But also your gut microbiome.”
The gut microbiome plays a far more crucial role in heart health than previously understood. Dr. Jamnadas notes, “The biggest difference between you and your outer environment is actually your gut, not outside your skin. It’s actually the gut.
When the gut microbiome is disrupted (whether by poor sleep, frequent time zone changes, or other factors), it creates a cascade of problems. A leaky gut allows lipopolysaccharides and other inflammatory molecules to enter the bloodstream, triggering inflammation throughout the body. This inflammation directly impacts the vagus nerve, which controls the balance between your sympathetic (fight or flight) and parasympathetic (rest and digest) nervous systems.
Dr. Jamnadas has observed this connection repeatedly: “I see a lot of young women in their 30s and 20s who come to me with tachycardia. They have a rapid heartbeat all the time, and especially when they stand up… When they come to me, I find out that it’s actually the gut. I fix their gut, and the tachycardia gets better. Because by fixing the gut, I’m fixing the vagus nerve. By fixing the vagus nerve, the heart rates come down.”
Fasting: The Ancient Solution to Modern Heart Disease
While calorie restriction and fasting might seem similar, Dr. Jamnadas explains they produce vastly different physiological responses. “When you cut down on calories, the body senses that this caloric deficit, the metabolic rate changes, actually slows down. And the body will start breaking down everything, muscles included. So you lose fat and you also lose muscles.”
Fasting, on the other hand, operates on a different principle: “Fasting is, I’ve put on fat, now I’m going to take it out of the bank… In the first 12 hours of a fast, you take out all the glucose in the form of glycogen from your muscles and your liver. After 12 hours, you start pulling the fat out. And the first place the fat comes out of is going to be visceral fat.”
Why does this matter? Visceral fat, the fat that accumulates around your organs and in your belly, is highly inflammatory. “If I did a biopsy of your visceral fat versus a biopsy of, let’s say, a fat from on your buttock, two different types of fat. One is full of inflammatory molecules… One is producing interleukin-6 and tumor necrosis factor, and this other fat is not.”
Dr. Jamnadas describes treating a woman with a supervised 72-day fast: “Diabetes, gone. Blood pressure, normalized. Weight loss, tremendous weight loss. I think she lost about 55 or 60 pounds.” He also mentions a male patient who fasted for 183 days, going from 400 pounds to 210 pounds, and remarkably, “when he walked into the office, you would not recognize that he’s just lost all this weight because he did not look like skin on top of bones.”
The benefits extend beyond weight loss. Fasting triggers numerous beneficial processes:
1. Ketone production: After 12 hours of fasting, your body starts producing ketones from fat. “Ketones are actually a cleaner fuel for the body,” producing fewer damaging reactive oxygen species.
2. Brain-derived neurotrophic factor (BDNF): This causes you to “become smarter, you’re growing new cells, your reflexes are better, your visual acuity is better.”
3. Stem cell mobilization: “When you break your fast, you get a surge of stem cells coming out of your bone marrow.” This boosts immunity and produces progenitor cells that repair blood vessels.
4. Growth hormone production: “The fastest way and the best way to actually increase your growth hormone production is to do intermittent fasting.”
5. Autophagy: Your cells recycle redundant organelles, producing more efficient mitochondria and removing toxins.
For practical implementation, Dr. Jamnadas recommends starting with a 12:12 fasting window (12 hours fasting, 12 hours eating) for 2-3 weeks, then progressing to 18:6 (18 hours fasting, 6 hours eating). During fasting periods, he allows water, black tea, black coffee, and green tea with no calories.
However, he emphasizes cycling in and out of ketosis: “You don’t want to be in ketosis all the time because that’s not what… our physiology was made for.” For healthy maintenance, he recommends at least one 36-hour fast per month.
Building Muscle While Fasting: Timing Is Everything
Contrary to popular belief, fasting doesn’t have to mean muscle loss. In fact, Dr. Jamnadas argues it can enhance muscle building: “You will find that you will put on more muscle, and you will retain more muscle as well, because you have higher growth hormone.”
The key is timing and the type of exercise. “When should you exercise when you’re fasting? At the peak of your fast. So if I’m going to break my fast at 6 p.m., I tell patients to go out to the gym at 4 o’clock in the afternoon.”
For exercise type, Dr. Jamnadas recommends resistance training and HIIT over prolonged aerobic activity during fasted states: “When it comes to the training that I’m talking about in a fasting state, I like resistance training. So in resistance training, that glucose issue is not going to become a problem.”
The Modern Toxin Crisis Hidden in Plain Sight
Beyond diet and exercise, Dr. Jamnadas identifies a growing threat to heart health: environmental toxins. “A toxin is a molecule that should not be in your body. You should not have been exposed to it.”
The list is extensive: pesticides, herbicides, plastics, forever chemicals (PFAS), BPA, mold, and heavy metals. “These chemicals all disrupt our metabolism in our body,” he explains. Many are estrogen receptor disruptors that cause inflammation.
The mold epidemic deserves special attention. “Almost 70% of homes these days have some form of mold toxicity in them, either from previous water damage or exposure.” The problem? “Mold can come in and then become part of your microbiome… you’re re-inoculating yourself over and over again with this mold.”
Dr. Jamnadas has observed direct connections between mold exposure and heart disease: “When I get rid of the mold, all of a sudden, I’m noticing that the patients are not only feeling better, but the rate of progression of coronary artery disease flattens off.”
When evaluating patients, he looks at the gut’s ability to detoxify: “When the gut is not working properly, you’re going to be more prone to toxicity because the gut bacteria normally grab a lot of those things and take them out in your stools.”
Foods You Thought Were Healthy That Are Destroying Your Heart
Dr. Jamnadas challenges several conventional health foods:
Calcium Supplements: “Calcium supplements actually increase the risk of cardiovascular events. Calcium supplements should not be taken. I stop all calcium supplements on all my cardiac patients.” The real problem isn’t calcium deficiency but lack of vitamin D3 and K2, which help the body properly utilize calcium.
Research supports this concern. Some large observational studies suggest that high-dose calcium supplements (especially above 1,000 milligrams a day from pills) may increase the risk of heart attack and stroke. Dr. Jamnadas particularly notes young women in their 30s with osteopenia despite taking calcium supplements, drinking calcium-fortified milk and orange juice, and living in sunny Florida. The solution? “You need D3 and K2. That’s what you need.”
Coffee: Good or Bad for Your Heart?
Coffee receives a nuanced evaluation. Moderate consumption (1-2 cups daily) can be beneficial, but not for the reasons you might think. “Coffee is good… not because of the caffeine,” Dr. Jamnadas clarifies. “Coffee has a lot of soluble fiber in it, so there is some soluble fiber in it, and it has polyphenols.”
These compounds feed beneficial gut bacteria, which produce postbiotics that reduce leaky gut and inflammation and protect the vagus nerve.
However, excessive caffeine poses problems. “Caffeine is very similar to the adrenaline molecule… You’re living in a state of existential threat constantly.” When Dr. Jamnadas sees patients drinking six cups of coffee daily, he considers “that’s toxicity.” The sweet spot? Keeping consumption under 600 milligrams of caffeine per day to avoid raising blood pressure, triggering arrhythmias, and stressing the heart.
Heart Palpitations: When to Worry and What They Really Mean
Heart palpitations can be frightening, but understanding when they’re dangerous versus benign is crucial. “If you have underlying structural heart disease, let’s say you have blocked arteries, let’s say you have a cardiomyopathy, a valvular disease, and you’re having an arrhythmia, which is palpitations, that is definitely life-threatening.”
However, for otherwise healthy individuals, palpitations usually indicate “an imbalance of your sympathetic and parasympathetic nervous system. You’re too stressed… you have too little parasympathetic.”
Causes can include:
– Excessive caffeine consumption
– Over-exercise (as discussed earlier)
– Leaky gut affecting the vagus nerve
– Poor lifestyle choices
Dr. Jamnadas has successfully treated many cases by addressing the root cause: “I fix their gut, and the tachycardia gets better. Because by fixing the gut, I’m fixing the vagus nerve.”
The Vagus Nerve: Your Body’s Master Controller
The vagus nerve emerges as a central player in heart health. “Cutting down on sleep is going to affect your entire physiology in your body and your repair processes and your vagus nerve,” Dr. Jamnadas explains.
When functioning optimally, a healthy vagus nerve provides:
– Faster healing
– Less coronary disease
– Lower blood pressure
– Reduced blood clotting tendency
– Lower inflammatory markers
– Better cholesterol profiles
The vagus nerve can be supported through three pathways:
1. Gut health: “When you fix the gut, your vagus nerve will be able to work more efficiently.”
2. Nutritional supplements: “You need DHA and omega-3 to make the vagus nerve work optimally.” Dr. Jamnadas notes that 50% of the population is deficient in omega-3.
3. Direct vagus nerve “hacking”:
– Breathing exercises: “Breathe in to the count of four, breathe out to the count of eight” for about 10 minutes daily
– Eye movements: Looking right, left, up, down, and in circles stimulates the vagus nerve
– Cold exposure: Ice packs on the front of the neck
– Humming or singing: Creates electrical impulses in the vagus nerve
– Laughing: The diaphragmatic movement stimulates the vagus nerve
– Gentle eyeball massage or cold water on eyeballs
The Valsalva Maneuver: An Emergency Tool for Your Heart
Dr. Jamnadas describes a simple technique that can help during episodes of rapid heart rate: “The Valsalva is when you breathe in and then you breathe out, but don’t let the air out. And you’re straining. And that straining compresses the thoracic cavity, but also the abdominal cavity and stimulates the vagus nerve.”
This technique has been found to be “very, very helpful” in managing acute episodes of palpitations or tachycardia.
The Perfect Diet for a Healthy Heart
After decades of treating heart disease, Dr. Jamnadas offers clear dietary guidance centered on reducing inflammation and supporting gut health:
What to Eat:
– 30-40 different types of vegetables per week (including spices)
– Real, unprocessed foods with fiber intact
– Eggs (for protein)
– Kefir (for vegetarians, with limited berries)
– Foods rich in omega-3 fatty acids
– 85% cacao chocolate (contains soluble fiber and polyphenols)
– Variety of fiber sources to foster different bacterial species
What to Avoid:
– Processed foods (fiber removed, extended shelf life)
– Frequent eating (aim for time-restricted feeding)
– Excessive carbohydrates and sugars
– Calcium supplements (unless directed by a doctor addressing specific deficiency)
– Excessive fruit
– White rice (due to arsenic content)
Supplementation:
– Vitamin D3 (for calcium absorption and bone health)
– Vitamin K2 (prevents calcium deposits in arteries)
– Omega-3 (DHA specifically, for vagus nerve function)
– Electrolytes during fasting (Celtic salt or LMNT)
– Probiotics, particularly spore-based probiotics like Bacillus coagulans
The timing matters as much as the content. Dr. Jamnadas emphasizes that “fasting is supposed to be a normal part of your existence. That’s the way you were designed.”
What Tests Should You Get Done?
For anyone over 30 concerned about heart health, Dr. Jamnadas recommends specific screening:
1. Coronary Calcium Score: “If your coronary calcium score is zero, you have no calcium, then you are in a good place. If you have coronary calcium, you need to go see a good cardiologist that’s going to do a prevention program because it means you already have atherosclerosis (hardening of the arteries).”
2. Comprehensive Inflammation Panel: Dr. Jamnadas orders a Cleveland Heart Labs blood test to look for inflammatory markers, including:
– Interleukin-6
– Tumor necrosis factor
– CRP (C-reactive protein) levels
– Small dense LDL particles
3. Insulin Level Testing: This is crucial and often overlooked. “We have a great opportunity here to actually start screening these patients with insulin levels very early on. But most doctors don’t have the ability or knowledge to do the insulin level testing, but it should be done.”
Dr. Jamnadas invested in a machine for his office specifically to measure insulin levels because “it’s all about insulin when it comes to the metabolic derangement.”
4. Gut Microbiome Evaluation: Stool samples to assess gut health and bacterial balance
5. Toxin Testing: Blood and urine samples to check for heavy metals, pesticides, herbicides, and mold toxicity
6. LDL Sub-fractionation: Not just total cholesterol, but whether you have small, dense LDL particles (which are inflammatory) versus large, fluffy LDL particles (which are benign)
The key insight? “There’s no such thing as essential hypertension,” meaning high blood pressure without a cause. “There’s always a cause. Either you have sleep apnea or you have hyperinsulinemia.” By identifying and addressing root causes rather than just treating symptoms, many patients can reverse their cardiovascular risk.
The Real Story: A 28-Year-Old’s Heart Attack
Dr. Jamnadas shares the story of his youngest heart attack patient to illustrate how modern lifestyle factors create the perfect storm for heart disease. At just 28 years old, this patient arrived with a full-blown heart attack, one coronary artery completely clogged with a blood clot.
What had he done wrong? “Number one, he was overweight. But he wasn’t just overweight. The overweight was all in his belly. And he had a fatty liver. And he had what is known as visceral fat. He was not a diabetic, but he was a pre-diabetic. That means he had a lot of insulin in his body.”
This patient’s glucose levels appeared normal to his family doctor. His hemoglobin A1c test was fine. But “that patient had a very high insulin blood level.”
This case exemplifies the critical ten-year window before diabetes diagnosis: “By the time you make a diagnosis of diabetes… you’ve already had 10 years of hyperinsulinemia… by the time you’re a diabetic and you come and see Dr. J in his cardiac clinic, you already have coronary artery disease.”
The solution? Early screening with insulin level testing and aggressive lifestyle intervention before reaching diabetic status.
Conclusion: Prevention Is Everything
Dr. Jamnadas’s message is clear and hopeful: heart disease is largely preventable through lifestyle modifications. The cornerstones are:
1. Manage insulin through intermittent fasting and reduced meal frequency
2. Incorporate appropriate exercise (resistance training, HIIT, and moderate aerobic activity)
3. Prioritize seven hours of quality sleep nightly
4. Support gut health through diverse vegetable intake and probiotics
5. Reduce environmental toxin exposure (mold, pesticides, plastics)
6. Support vagus nerve function through breathing exercises, omega-3 supplementation, and gut health
7. Get appropriate screening tests, particularly insulin levels and coronary calcium scores
8. Address inflammation at its root causes rather than just treating symptoms
As Dr. Jamnadas emphasizes, “We’re transforming the whole definition of the causes of coronary artery disease. We have been so myopic in our definition of what causes coronary artery disease. With everything, your entire lifestyle, mental, physical, eating, everything will affect your coronary arteries.”
The power to prevent heart disease lies not in pharmaceutical interventions alone, but in understanding and working with your body’s natural physiology, particularly the ancient practice of fasting and the modern understanding of the gut-brain-heart axis. By addressing these fundamental factors, we can reclaim our cardiovascular health and potentially reverse decades of damage.

Leave a Reply
You must be logged in to post a comment.