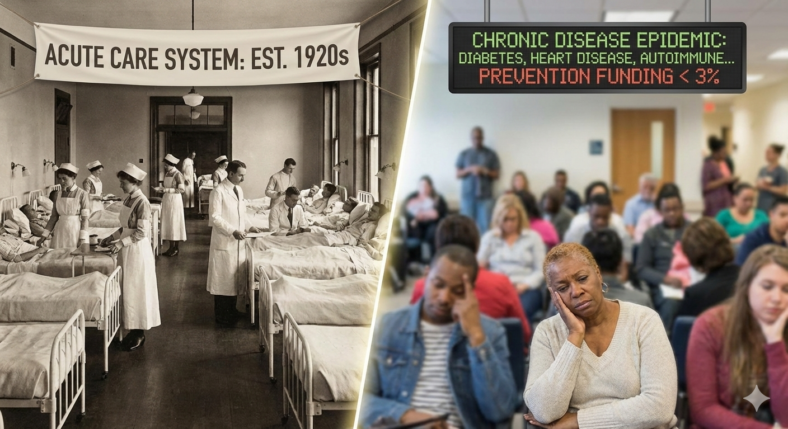
Here’s an uncomfortable truth: the medical system you rely on wasn’t designed to keep you healthy. It was designed to treat you when you’re sick.
This isn’t a conspiracy theory or an indictment of doctors’ character. It’s simply the result of how medicine evolved over the past century. The system that developed to fight infectious diseases and acute injuries, while remarkably successful at those goals, never fully adapted to the chronic disease epidemic we face today.
Understanding why this happened, and what you can do about it, could be the most important health knowledge you gain this year.
How We Got Here: The Evolution of Modern Medicine
To understand the current state of healthcare, we need to look at where we came from. Dr. Peter Attia, a longevity expert, describes the evolution of medicine in three phases.
Medicine 1.0 was everything that existed before we really understood the science of medicine. For most of human history, we had no idea why people got sick or why people died or what an infection meant. We thought these were plagues from the gods or things of that nature.
Then a couple of revolutionary things happened in the past few hundred years. First was the invention of the scientific method itself: the ability to make an observation about something in the world, formulate a hypothesis about why it’s happening, and then design an experiment to test it. That’s a creation. We had to figure that out.
This led to Medicine 2.0, the current system we have today. Medicine 2.0 brought us antibiotics, vaccines, surgical techniques, and treatments for infectious diseases. The invention of antibiotics was credited as a chief reason the Allies won World War II. Medical trust was at its height post-World War II, and for good reason: the medical system had developed remarkable tools to fight acute illness and injury.
The problem? Today, most people are going to die from cardiovascular disease, cancer, dementia, or complications of diabetes. And on one hand, that’s a sign of progress. It means we’re living long enough to die from those things. But we’ve made scant progress against those things. In fact, if you go back and strip out the top eight causes of infectious death or communicable death, our life expectancy today is not much better than it was in the 1800s.
The medical system that evolved to treat acute infectious disease was never redesigned to prevent chronic disease.
Why the System Treats Instead of Prevents
Dr. Sara Gottfried, a precision medicine expert, doesn’t mince words: “Conventional, mainstream, modern medicine, I believe, is broken. I feel like there are so many people who are failed by our current medical system, especially people with chronic disease, things like diabetes, autoimmune disease.”
She explains the fundamental problem: “With mainstream medicine, generally what happens is that you develop a condition, say a high cholesterol, and you get treated with a pharmaceutical, say a statin. And what we know is that we have to treat about 100 to 200 people for one person to benefit.”
But why does the system work this way? Dr. Gottfried identifies a key issue: “It’s not about optimal health. It’s centered around, okay, heart disease is number one killer. How do we help people prevent it? Oh, lifestyle medicine prevents 70% of it? Well, we’re not going to do that because we can’t make money off of it. There’s no profit motive. So, we’re going to focus instead on these pharmaceuticals.”
Let that sink in: 70% of the diseases we’re facing right now are utterly preventable with lifestyle medicine. Yet the system focuses on pharmaceutical intervention after disease develops.
The Numbers Are Stark
The data reveals just how little emphasis the medical system places on prevention:
According to research discussed on the a16z Podcast, if you look at the pie charts for a number of government agencies, including the National Cancer Institute and NIH in general, preventative medicine is in the 1 to 5% of the pie chart. Yet its payback is enormous.
In 2020, total U.S. healthcare expenditure was $4.1 trillion, which is around $12,500 per person. But of that, only around $363 was spent on prevention. That’s less than 3% spent on preventing disease versus 97% spent treating disease after it develops.
It’s Not Malicious, It’s Structural
It’s crucial to understand: this isn’t about bad actors or evil intentions. It’s about how systems evolve and where incentives lie.
Dr. Daniel Lieberman, a Harvard evolutionary biologist, explains it this way: “You don’t see a doctor in our medical system until you get sick, right? And then you get pills to lower your blood pressure and pills to lower your cholesterol. But these aren’t, well, those, some of them can be preventative, but to a large extent, most of medical treatments are treating the symptoms of diseases after they occur.”
He continues: “And of course we should do that. We should alleviate pain, we should alleviate suffering. We should try to decrease people from dying from all kinds of diseases. But wouldn’t it be better if we actually prevented those diseases in the first place? We would have a much more effective medical system.”
The healthcare system also faces misaligned incentives. As discussed on the a16z Podcast, health providers like hospital systems and doctors’ offices don’t really see patients as their own customers because patients generally aren’t paying for their care; the insurance company is. So they’re optimizing for the insurance company instead of the patient.
Dr. Tom Frieden, former director of the CDC, points to a successful counter-example: Kaiser Permanente. Years ago, Kaiser realized that if they helped their members reduce their blood pressure, their members would have fewer heart attacks and strokes, would live longer, they’d get more money, and their members would be healthier. When they realized that, their control rate, the proportion of all people who had their blood pressure controlled, was only 40%. Today, it’s 90%. The rest of the country? 45%. They do twice as well as the rest of the country because the incentives are aligned.
Dr. Frieden summarizes the broader problem: “We need to change the incentives so we’re not incentivizing sick care. We’re incentivizing health care.”
Prevention Is a Hard Sell
Even within medical practice, prevention faces an uphill battle. Dr. Gottfried notes: “Prevention has been a hard thing to sell. It’s, you know, a lot of people just don’t want to invest in prevention. And yet, I take care of people who are in this continuum from a state of health, often to a state of pre-disease, like pre-diabetes, as an example. And if they don’t do something about it, they then move on to diabetes. So I like to intervene there as early as possible to reverse disease. And most of that is lifestyle.”
Why is prevention hard to sell? Several reasons:
1. Immediate costs, delayed benefits: Prevention requires effort and investment now for benefits that might not materialize for decades.
2. No profit motive: As discussed, there’s limited financial incentive for pharmaceutical companies or healthcare systems to focus on prevention when treatment is far more profitable.
3. Lack of drama: Successfully preventing a heart attack means nothing happens. There’s no dramatic save, no obvious success to point to.
4. Individual responsibility: Prevention requires sustained personal effort: eating well, exercising, managing stress. It can’t be outsourced entirely to a pill or procedure.
The Good News: Change Is Coming (Slowly)
Despite these structural barriers, a paradigm shift is underway. Dr. Attia calls it Medicine 3.0, and it involves real prevention.
The key principles of Medicine 3.0:
1. True Prevention: Taking steps at prevention very early in life, long before disease manifests.
2. Personalization: You can’t just do medicine by numbers. You can’t just say the same thing to everybody. While certain things make absolute sense across the board, such as sleep and exercise, the way you might use medications or interventions has to be much more tailored to an individual.
3. Risk Assessment: Understanding not just the risk of doing something, but the risk of not acting, and considering risk over appropriate time horizons (decades, not just the next 10 years).
4. Root Causes, Not Just Symptoms: Dr. Mark Hyman and other functional medicine practitioners are pioneering approaches that address underlying causes rather than just suppressing symptoms.
Dr. Gottfried describes this shift as precision medicine: “We understand you as an individual, we look at your genomic blueprint, we look at your biomarkers, we look at your wearables data, to determine experiments where you serve as your own control and figure out what’s going to be the most effective for you, depending on what your goals are.”
What You Can Do: Take Control
Given that the medical system isn’t optimized for prevention, what can you do?
1. Accept Responsibility for Prevention
Recognize that doctors are primarily trained and incentivized to treat disease, not prevent it. While you should absolutely use the medical system for acute care, screenings, and treatment when needed, don’t expect your doctor to be your primary partner in prevention.
Prevention is your job.
2. Focus on Lifestyle Medicine
Remember: 70% of chronic diseases are preventable with lifestyle changes. The foundations are unsexy but powerful:
Sleep: Prioritize 7-9 hours of quality sleep per night. This is non-negotiable for health.
Exercise: Both cardiovascular exercise and strength training. Movement is medicine.
Nutrition: Focus on whole, unprocessed foods. Minimize added sugars and ultra-processed foods. Prioritize protein and fiber.
Stress Management: Chronic stress drives disease. Modern life presents stress at levels that we were never meant to deal with. Develop practices like breathwork, meditation, or other stress-reduction techniques.
Social Connection: Loneliness and social isolation are as harmful to health as smoking. Invest in relationships.
3. Educate Yourself
You are living in an unprecedented era of access to health information. Learn about your body, how it works, what drives disease, and what promotes health. Be a critical consumer of health information, but don’t be passive.
4. Be Proactive, Not Reactive
Don’t wait until you have a diagnosis to care about your health. The time to prevent diabetes is before you develop pre-diabetes. The time to prevent heart disease is in your 30s and 40s, not after your first heart attack.
Get baseline measurements: blood work, body composition, fitness levels. Track them over time.
5. Find Practitioners Who Think Preventively
While the system isn’t optimized for prevention, individual practitioners exist who think differently. Look for doctors who:
– Spend time understanding your goals and context
– Talk about prevention, not just treatment
– Consider lifestyle interventions first
– Are willing to look at root causes
– Take a personalized approach
Functional medicine practitioners, longevity-focused physicians, and precision medicine doctors are growing in number.
6. Accept That This Will Require Effort
There is no pill for prevention. There’s no shortcut. Taking control of your health requires sustained effort: preparing healthy meals, prioritizing sleep when you’d rather stay up, exercising when you’d rather not, saying no to tempting but unhealthy options.
This is hard. That’s why most people don’t do it. But the payoff is measured in years added to your life and life added to your years.
7. Start Now
The best time to start was 20 years ago. The second best time is today. Every day you invest in prevention is a day you’re building a healthier future self.
The Bottom Line
The medical system evolved to treat infectious diseases and acute injuries, and it does those things remarkably well. But it was never redesigned to prevent the chronic diseases that now kill most of us.
This isn’t through mal-intent. It’s the result of how medical understanding evolved, how financial incentives developed, and how the system was structured.
Things are changing, but slowly. Medicine 3.0, precision medicine, functional medicine: these are all movements toward a more preventive, personalized approach. But they’re still the exception, not the rule.
In the meantime, you can’t afford to wait. You can’t outsource prevention to a system that wasn’t designed for it.
Dr. Frieden offers this powerful summary: “Most of the illness that we see can be prevented today. It can be prevented if we as a community get together and do what’s proven to work.”
The knowledge exists. The tools exist. What’s required now is for individuals to take ownership of their health, to recognize that prevention is primarily their responsibility, and to invest the time and effort required.
Your doctor can be an ally in this journey. The medical system can provide important services, screenings, and interventions when needed. But the day-to-day work of staying healthy, the thousands of small decisions that determine whether you develop chronic disease or not, that’s on you.
Take control of your own health. Because no one else is going to do it for you.
References
1. The Diary Of A CEO with Steven Bartlett: “Dr. Sara Gottfried on Menopause, Hormones, and Why Modern Medicine Is Broken” https://primates.life/menopause-expert/
2. The Diary Of A CEO with Steven Bartlett: “Daniel Lieberman: Our Comfortable Lives Are Causing Cancer” https://primates.life/worlds-no-1-exer/
3. The Diary Of A CEO with Steven Bartlett: “Peter Attia: The Life Extension Doctor” https://primates.life/the-life-extens/
4. Guy Kawasaki’s Remarkable People: “Why Prevention Is the Best Medicine with Dr. Tom Frieden” https://primates.life/why-prevention-/
5. a16z Podcast: “What’s in the Water at the George Church Lab” https://primates.life/a16z-podcast-wh/
6. a16z Podcast: “The Longevity Imperative: Redefining the Way We Age” https://primates.life/the-longevity-i/
7. a16z Podcast: “It’s Time to Build in Healthcare” https://primates.life/its-time-to-bui/
8. My First Million: “The Dark Story Behind Ozempic’s $500B Business Empire” https://primates.life/the-dark-story-/

Leave a Reply
You must be logged in to post a comment.